A Damning Review of the Justifications for Puberty Blocker Use in the U.K.
NEWS
Oxford professor Micheal Biggs has been vocal in criticizing the protocols for treating gender dysphoric minors at the Gender Identity Development Service in the United Kingdom. He has completed a review of the decisions that have been made by the Tavistock clinic around the use of puberty blockers and a move towards an affirmative model titled “The Tavistock’s Experiment with Puberty Blockers.”
The first quote provides the history of the use of puberty blockers for gender dysphoria:
In 1994 a 16-year-old girl who wished to be a boy, known to us as B, entered the Amsterdam Gender Clinic. She was unique for having her sexual development halted at the age of 13, after an adventurous paediatric endocrinologist gave her a Gonadotropin-Releasing Hormone agonist (GnRHa). Originally developed to treat prostate cancer, these drugs are also used to delay puberty when it develops abnormally early: in girls younger than 8, and boys younger than 9. The endocrinologist’s innovation was to use the drug to stop normal puberty altogether, in order to prevent the development of unwanted secondary sexual characteristics—with the aim of administering cross-sex hormones in later adolescence. Dutch clinicians used B’s case to create a new protocol for transgendering children, which enabled physical intervention at an age far below the normal age of consent (Cohen-Kettenis and Goozen 1998).
His review is not positive:
This paper describes the origins and conduct of this study and scrutinizes the evidence on its outcomes. It draws on information obtained by requests under the Freedom of Information Act to the Tavistock, to the NHS Health Research Authority, and to University College London (UCL). I will argue that the experimental study did not properly inform children and their parents of the risks of triptorelin. I will also demonstrate that the study’s preliminary results were more negative than positive, and that the single published scientific article using data from the study is fatally flawed by a statistical fallacy. My conclusion is that GIDS and their collaborators at UCL have either ignored or suppressed negative evidence. Therefore the NHS had no justification for introducing the Dutch protocol as general policy in 2014
The paper addresses the fact that the hormone blocker protocol has been called reversible and that this has not actually been proven and is very likely not true. GHQ covers the many statements by affirmative model advocates that blockers are “fully reversible” and the actual serious consequences of blockers here.
The paper also describes the reality that the blocker to cross-sex hormone protocol stunts genital growth:
One further absence deserves emphasis. The 2005 Symposium had noted the paradox that blocking a boy’s puberty left him with stunted genitalia, which were then not sufficient to transform into a pseudo-vagina.
This necessitates a more drastic vaginoplasty surgery. We cover the ramifications of this protocol.
Biggs goes on to criticize the Tavistock professionals:
Three years after the experiment began, Carmichael announced success to the tabloid press. “Now we’ve done the study and the results thus far have been positive we’ve decided to continue with it” (Mail on Sunday, 17 May 2014). Her statement was at best misleading.
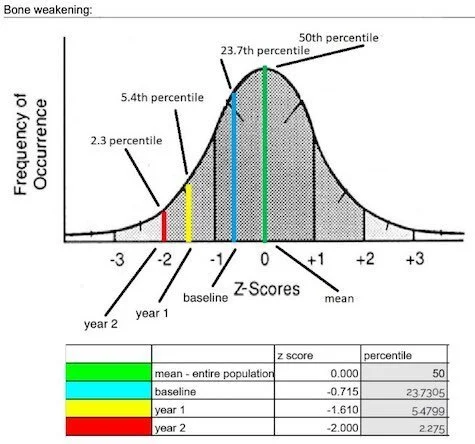
Biggs on bone density, something the GHQ website covers here:
The authors state reassuringly that bone density did not decline in absolute terms. This is misleading, because growing children need density to increase (Laidlaw 2018). The abstract acknowledges that the children experienced a decline relative to the norm for their age group, and this decline was especially marked for girls. By year three, the average girl on GnRHa had lower bone density than 97.7% of the population in her age group. Surely this raises serious concerns?
A graph:
He describes on the psychological outcomes (particularly in females who are coming out as trans in unprecedented numbers) and what appears to be an intention to spin them in the most positive way possible, despite some negative findings:
Diligent searching has uncovered unpublished results on the psychological effects. Most revealing is an appendix to Carmichael’s report to the Tavistock’s Board of Directors (GIDS 2015).4 It tracks 30 of the children on triptorelin, measuring changes after one year of the drug regime; presumably the remaining 14 subjects had not completed their first year on the drug.5The text is sometimes internally inconsistent and occasionally contradicts the tabulated figures, suggesting that the appendix was prepared in haste. But we can summarize those changes that were reported as statistically significant (p-value < .05). Only one change was positive: “according to their parents, the young people experience less internalizing behavioural problems” (as measured by the Child Behavior Checklist). There were three negative changes. “Natal girls showed a significant increase in behavioural and emotional problems”, according to their parents (also from the Child Behavior Checklist, contradicting the only positive result). One dimension of the Health Related Quality of Life scale, completed by parents, “showed a significant decrease in Physical well-being of their child”. What is most disturbing is that “a significant increase was found in the first item ‘I deliberately try to hurt or kill self’” (in the Youth Self Report questionnaire). Astonishingly, the increased risk of self-harm attracted no comment in Carmichael’s report. Given that puberty blockers are prescribed to treat gender dysphoria, it is paradoxical that “the suppression of puberty does not impact positively on the experience of gender dysphoria” (measured by the Body Image Scale). When differentiated by sex, the impact was positive for boys on one aspect of body image, but negative for girls on two aspects.
Another problematic example:
The abstract proclaims that “adolescents receiving also puberty suppression had significantly better psychosocial functioning after 12 months of GnRHa ... compared with when they had received only psychological support” (Costa et al. 2015: 2206). The literature treats this article as providing evidence in favour of puberty blockers (e.g. Butler et al. 2018; Heneghan and Jefferson 2019). But the abstract is misleading: the analysis actually failed to detect any difference between children who were given GnRHa and those who were not
The paper ends with a suggested ban on hormone blockers and more extensive research:
What, then, is to be done? Richard Byng (2019) recently demanded a moratorium on the use of GnRHa for children suffering from gender dysphoria until there is robust evidence that this drug regime is safe and effective. A team of independent researchers must be given access to all the data from the 2011 experiment. They will need expertise in statistics, psychiatry, and endocrinology; most importantly, they must have no vested interests in the promotion of GnRHa. Given that this experiment has been used since 2014 to justify the provision of these drugs to children under the NHS, the outcomes of this experiment—on all the physical and psychological measures that were collected—must be published urgently.
Update 08/18/19: Adding information on late puberty and lack of bone density “Teenagers who identify as transgender taking powerful ‘puberty blocker’ drugs ‘may suffer from weaker bones in the future’”
Update 10/22/19: The study has been cleared of ethics concerns by the Health Research Authority but criticisms continue.
REFERENCES:
Adams, S. (2019, August 17). Teenagers who identify as transgender taking powerful ‘puberty blocker’ drugs ‘may suffer from weaker bones in the future.’ Daily Mail. Retrieved from https://www.dailymail.co.uk/debate/article-7368017/Teenagers-identify-transgender-taking-puberty-blocker-drugs-suffer-weaker-bones.html
Biggs, M. (2019, July 29). The Tavistock’s Experiment with Puberty Blockers. Department of Sociology and St Cross College, University of Oxford. Retrieved from http://users.ox.ac.uk/~sfos0060/Biggs_ExperimentPubertyBlockers.pdf
We do not have open comments on the Gender Health Query website. But that doesn’t mean we aren’t interested in what you have to say. If you have a comment, blog post idea, or any other feedback, we would be interested if the information can be supported by science research, an informed opinion, real-world observations, or personal experiences. Please contact us.